Before Surgery
 Bariatric surgery will require major lifestyle changes, even before your surgery. Your physician may ask you to:
Bariatric surgery will require major lifestyle changes, even before your surgery. Your physician may ask you to:
- Stop smoking several months prior to your surgery. Nicotine decreases blood flow, prevents healing after surgery, increases your risk of infection or other complications.
- Increase your activity. Aim for 30-60 minutes of walking or other aerobic activity daily to build strength.
- Improve your nutrition by adding daily vitamins and protein supplements to help your body heal after surgery and prevent malnutrition.
- Eliminate the use of alcohol.
- Modify your use of medications.
- Avoid ibuprofen or NSAIDs for the remainder of your life.
Please ask your physician about any additional steps you should take before your surgery.
Surgery
Our surgeons perform two types of bariatric surgery:
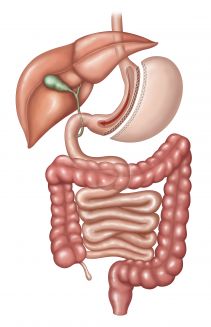
Gastric Sleeve (Gastrectomy). In this procedure, a portion of your stomach is removed, creating a smaller, narrower stomach called a “sleeve.” After surgery, the stomach resembles a banana, restricting how much food may be eaten. Food will still be absorbed normally in your intestines. This surgery typically results in decreased hunger sensations due to hormonal changes. Weight loss occurs fairly rapidly.
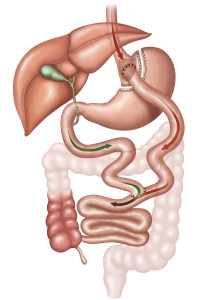
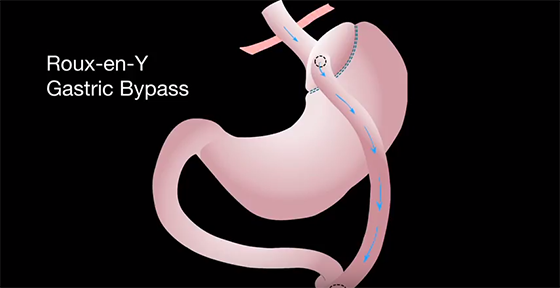
Roux en Y Gastric Bypass. During this surgery, the most common gastric bypass procedure, your stomach is divided to create a small pouch about the size of your thumb. This causes you to feel full after only a few bites of food. Your intestine is divided and reattached to your stomach so that the outlet from the pouch empties into the small intestine, causing food to bypass approximately 150 cm of your intestine. This procedure restricts the amount of food that may be eaten, as well as reduces the amount of nutrients and calories that are absorbed, resulting in rapid weight loss.
In most cases, bariatric surgery is performed laparoscopically, but our surgeons can perform both open surgery and minimally invasive procedures.
Open surgery. With open surgery, your physician will make an incision large enough so he or she can see and touch your internal organs while operating.
Minimally invasive surgery. Minimally invasive surgery is performed with traditional laparoscopy or robot-assisted surgery using the da Vinci Surgical System.
• Laparoscopic surgery. Laparoscopic surgery requires only a few small incisions into which your surgeon will fit long, thin surgical instruments and a tiny camera. The camera will provide images to guide the surgeon during the procedure.
• Robotic surgery. Some laparoscopic surgeries may be performed using the da Vinci Surgical System. This robotic option gives your surgeon a magnified 3D high-definition view inside your body. The system also enables the surgeon’s hand movements to be translated into precise movements of small instruments inside your body.
After Surgery
- You will be encouraged to walk to prevent blood clots, muscle weakness and constipation.
- You will be placed on a liquid diet for several weeks.
- You may take one or two tablespoons of Milk of Magnesia for constipation.
- Ice may help to reduce the swelling for the first 48 to 96 hours. Then use heat to ease muscle soreness and relax tight muscles.
- A small amount of bleeding or drainage is expected from the wound during the first one or two days.
- You may shower one or two days after surgery, but avoid baths, hot tubs, soaking or swimming for at least two weeks.
- Always talk to your surgeon about weight restrictions and return-to-work options.
- You will be asked to see your surgeon in one to three weeks after surgery.
Call your surgeon right away if you have any of the following:
- Redness, pain or increased swelling or drainage at the incision site
- Fever of 100.4 degrees F. or higher, or shaking chills
- Fast pulse or increase in respiratory rate
- Persistent pain, nausea or vomiting
- Diarrhea beyond the first week
- Pain in your upper back, chest or left shoulder
- Persistent hiccups
- Confusion, depression or unusual fatigue
Dietary Instructions for Gastric Sleeve (Gastrectomy) Patients:
Fluids. When you leave the hospital, you will be on a clear liquid diet and given instructions about measuring your fluid intake daily. The goal is to drink at least 64 ounces every day by the third or fourth day after surgery. Continue this clear liquid diet until you are seen for your one-week follow-up visit with your surgeon.
Medications. Your physician may prescribe one or more of the following medications:
- Omeprazole (Prilosec) 20 mg daily. Open the capsule and mix the contents with a small amount of liquid to drink. This must be taken, as it is very important in helping your stomach heal after surgery. You will need to take this for 8 to 12 weeks.
- Hyoscyamine Sulfate (Levsin) 0.125 mg to be taken under the tongue to prevent esophageal spasms
- Hydrocodone or Roxicet for pain as instructed
- Ondansetron (Zofran) taken under the tongue for nausea
Weeks 1 and 2. You will be on a clear liquid diet for the first two weeks after surgery. You may have sugar free, non-caffeine, non-carbonated beverages such as water, flavored water, diluted juices, sugar-free Jello and broth.
Weeks 3 and 4. At this point, you may try a full liquid diet including tomato or V8 juice; tomato soup (diluted 1:1 with water or skim milk); low-fat, low-calorie strained cream soup; low-fat milk or yogurt without fruit. Continue to monitor your fluid intake to reach 64 ounces a day.
Weeks 5 and 6. You may now begin a puree diet using foods in your handbook. A few days after starting this diet, you should begin taking your supplements, as instructed by your physician. Make an appointment to see the dietitian and nurse coordinator before starting your solid food diet. Call 763.581-5355 to schedule these appointments.
Week 7. Seven weeks after surgery, you may begin solid foods. Remember to take very small bites about the size of a pea, and chew very well. You need to chew 25 to 35 times for each bite until food is of the consistence of applesauce. Do not drink with your meals. Wait 30 to 45 minutes after eating before drinking. Stop eating before you feel full. Meals should be a couple of tablespoons total per meal. Once this is routine, you may slowly eat up to ¼ cup at a meal by around three months after surgery. Continue to drink more than 64 ounces of fluid a day.
Dietary Instructions for Roux en Y Gastric Bypass Patients:
Fluids. When you leave the hospital, you will be on a clear liquid diet and given instructions about measuring your fluid intake daily. The goal is to drink at least 64 ounces every day by the third or fourth day after surgery. Continue this clear liquid diet until you are seen for your one-week follow-up visit with your surgeon.
Medications. Your physician may prescribe one or more of the following medications:
- Hyoscyamine Sulfate (Levsin) 0.125 mg to be taken under the tongue to prevent esophageal spasms
- Hydrocodone or Roxicet for pain as instructed
- Ondansetron (Zofran) taken under the tongue for nausea
Week 1. You will be on a clear liquid diet for the first week after surgery. You may have sugar free, non-caffeine, non-carbonated beverages such as water, flavored water, diluted juices, sugar-free Jello and broth.
Weeks 2 and 3. At this point, you may try a full liquid diet including tomato or V8 juice; tomato soup (diluted 1:1 with water or skim milk); low-fat, low-calorie strained cream soup; low-fat milk or yogurt without fruit. Continue to monitor your fluid intake to reach 64 ounces a day.
Week 4. You may now begin a puree diet using foods in your handbook. A few days after starting this diet, you should begin taking your supplements, as instructed by your physician. Make an appointment to see the dietitian and nurse coordinator before starting your solid food diet. Call 763.581.5355 to schedule these appointments.
Week 5. Five weeks after surgery, you may begin solid foods. Remember to take very small bites about the size of a pea, and chew very well. You need to chew 25 to 35 times for each bite until food is of the consistence of applesauce. Do not drink with your meals. Wait 30 to 45 minutes after eating before drinking. Stop eating before you feel full. Meals should be a couple of tablespoons total per meal. Once this is routine, you may slowly eat up to ¼ cup at a meal by around three months after surgery. Continue to drink 64 ounces of fluid a day.
Lifestyle Changes:
Bariatric surgery will help you lose weight, but it is important to make lifestyle changes for the best long-term outcome. After surgery, you will be asked to make the following changes:
- Avoid alcohol and tobacco.
- Increase your activity. Aim for 60 minutes of walking or other aerobic activity daily to build strength.
- Improve your nutrition by adding daily vitamins and protein supplements to help your body heal after surgery and prevent malnutrition.
- Eliminate the use of alcohol.
- Modify your use of medications if your physician recommends it. This may include changing to a crushable or liquid form, in some cases.
- Avoid ibuprofen or NSAIDs for the remainder of your life.
- Don’t drink liquids with your meals.
- Have yearly check-ups and lab tests for the remainder of your life.
- Avoid pregnancy for at least one to two years after surgery.
North Memorial Medical Center offers an integrated metabolic and bariatric surgery program to provide comprehensive care, management and planning for surgical weight loss for qualified patients. The program is a partnership with Specialists in General Surgery and headed by Jonathan C. Gipson, M.D., FACS. Visit North Memorial Bariatric and Metabolic Surgical Weight Loss for more information.
If you have additional questions, please contact us at 763.780.6699.
Videos
Laparoscopic Sleeve Gastrectomy information
Laparoscopic Roux En Y Gastric Bypass information
Overview of Bariatric Surgery by a Patient & Dr. Gipson